
Medication Reconciliation: One Large Pill to Swallow
How One Project is Making a Dent in One of Healthcare’s Toughest Problems
By Vickie Kamataris, RN CPHQ
At the Institute for Healthcare Improvement (IHI) Forum in December, 2009, a billboard-sized model of the IHI Improvement Map was erected outside the exhibit hall. The map lists core healthcare processes. Beside the map was a container of silver pushpins and a container of red pushpins. Summit participants were asked to insert a silver pin into one process they felt they had mastered and a red pin into that which they considered most difficult and problematic. The results, while not scientific, were obvious. Medication reconciliation is, without a doubt, one of healthcare’s toughest problems. At the time I was in the Measure Phase of a Lean Six Sigma DMAIC project leading a team to solve the Medication Reconciliation problem at a hospital in New York. I showed this photo to my team and they replied, “This is not news to us!” As I’m writing this we are in the final phase of the project, and this is the story of how we got there.
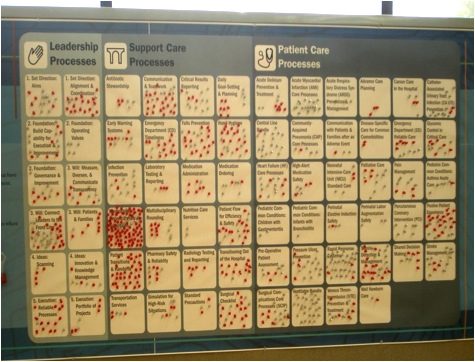
Snapshot of 2009 IHI Forum Improvement Map
Let’s Back Up a Few Months
A hospital system had just begun the launch of SystemCPI, our approach to deploying performance improvement methods in healthcare. Lean was to be used as the initial approach to improving hospital processes. Lean methods such as Value Stream Analysis (VSA) and Rapid Improvement Workshops (RIW) offer quick returns in a short timeframe. This works great early on to solidify leadership support and to generate organizational enthusiasm for the program. Six VSAs and multiple RIWs were completed during the first few months. The results were immediate and impressive. The deployment gained momentum and the excitement among leadership and staff was escalating. However, each of the inaugural VSAs had identified Medication Reconciliation as a barrier to achieving even greater breakthroughs.
Medication reconciliation errors, because the vital Xs or root causes are unknown, are better to be addressed using the Six Sigma DMAIC approach. One ProcessVSA immediately improved performance relative to HF core measures from 75% to 100% - excluding medication reconciliation errors. While overall performance improved markedly to a sustained 85%, medication reconciliation errors dragged performance down from 100%. Because of the complexity and urgency of this problem, the hospital’s leadership asked me to lead the project and work with a team to implement sustainable solutions.
Understanding the Problem
During the Define phase, the Medication Reconciliation DMAIC was chartered and a team was selected. Team members included nurses, pharmacists, and physicians. Other key stakeholders including HIM (Health Information Management) and Clinical Informatics were represented. The scope of the project was broad, including all patients admitted to the hospital and encompassing the entire patient experience, from pre-admission to the next point of care after disposition.
Moving into Measure, the baseline performance was unknown beyond CHF so a measurement system was designed and implemented. We randomly selected records of patients discharged from all patient care units, all DRGs, inpatients and outpatients. After we pulled all the data together for evaluation, baseline process capability was determined to be 40% or 600,000 Defects Per Million Opportunities (DPMO). At 1.25σ, a measure used in the Six Sigma world, medication reconciliation performance was even worse than predicted by the HF proxy.
.jpg)
Medication Reconciliation Sigma Level
Medication reconciliation is a highly complex process with more than 90 steps, 53% of which are non value-added, with many handoffs between functions and disciplines. A Cause and Effect Analysis identified hundreds of potential causes, or Xs. Statistical analysis verified that some presumed Xs did have a significant impact on medication reconciliation errors: number of home medications, high-risk medications, and patient level of consciousness. Other presumed Xs had little or no impact and were eliminated as causative factors: admitting unit, diagnosis-related group, disposition destination, care of the patient by a resident, number of prescribing providers, admitting and discharging physician and nurse, therapeutic drug interchanges, inpatient or outpatient status. One unexpected finding was the significant relationship between oversight by a hospitalist and medication reconciliation compliance.
Significant Causes of Error Insignificant Causes of Error Number of home medications Diagnosis-related group High risk medications Disposition destination Patient consciousness level Care of patient by a resident Number of prescribing providers Admitting and discharging physician / nurse Therapeutic drug interchanges Inpatient / Outpatient stat
Causes of errors found to be statistically significant during project.
Implementing Sustainable Improvements
The Improve phase focused on identifying and leveraging hospitalist practices, creating a Complex Medication Profile, and a process to manage patients meeting profile criteria. Innovation tools such as TRIZ were utilized by the team to create ‘outside the building’ solutions to seemingly impossible problems. The medication reconciliation process was simplified, a plan was developed to deal with constraints in the process, and many handoffs were eliminated. The use of technology to document and communicate medication-related information within and beyond the hospital was improved. Forms were re-designed according to user specifications and new standard procedures were implemented.
The results of an initial test of change were promising, but there were a few details that still had to be worked through with the team. While the scope of the test was narrow by design and patient census was unexpectedly low on the test unit, there were no medication reconciliation defects in the test population during the two-week test. Feedback from providers, nurses, and patients was overwhelmingly positive, with one staff nurse stating, “This is the first time I have ever participated in anything that actually improved patient care and made our job easier!” Lessons learned were incorporated and a second, far more comprehensive test of change has been designed and will occur during the first two weeks of August.
How to Pay for All of This?
The team’s analysis also revealed the need for a pharmacist review of Complex Med Profile patients at discharge and the team was faced with an even greater challenge: how to pay for pharmacist time and all these other changes to the medication reconciliation process!
Tune in to the next edition of this newsletter to find out the creative solution the team devised to add $1.3 Million in new revenues and pay for all the improvements needed! We’ll summarize the results of the second test of change and describe some of the ways that the hospital was able to solve one of healthcare’s toughest problems.
For more information on this article or to contact the Vickie directly, send an email to vkamataris@novaces.com.
Also in This Issue of the Newsletter
Performance Improvement Mistakes, Part 3: Get Leadership Buy-In


Follow Us: